Case: 40 year old female with fever and SOB
Neha Pradeep
MBBS 9th semester
Roll no: 99
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome .
I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan.
CASE:
A 40 year old female with complaints of fever since 20 days and shortness of breath since 3 days.
History of Presenting Illness:
Patient was apparently asymptomatic 20 days ago, when she developed a fever. Fever was insidious in onset and gradual in progression. Fever was associated with chills and rigors. Fever was intermittent. Evening rise of temperature was present. Relieved on taking medication. Fever was also associated with several episodes of vomiting. Vomitus was watery, non bilous, non projectile, non foul smelling and non bloodstained.
Patient also complained of shortness of breath since 3 days. Insidious in onset and progressive (Grade II to Grade IV). Not associated with orthopnea or PND or pedal edema. Since one day, patient has had SOB even on rest.
Patient has no complaints of cough, cold, seizures, headache, burning micturition, or suprapubic pain.
Past History:
Patient had a similar episode of fever, 4 months ago, was treated locally and resolved.
Patient has no past surgical history.
Patient is a known case of hypertension since 3 years, not on any medication. She was diagnosed on screening.
Not a known case of Diabetes, Tuberculosis, or Asthma.
Personal History:
Diet: Mixed
Appetite: Normal
Sleep: Inadequate, unable to fall asleep
Bowel and Bladder: Regular
Drinks Alcohol every day for the last 5 years. (90ml)
No smoking or allergies.
GENERAL EXAMINATION:
Patient is conscious, cooperative and coherent. Well oriented to time, place and person. Moderately built and moderately nourished.
Vitals: (at time of admission)
BP: 110/70 mmHg on left arm
Respiratory Rate: 24 cycles/min
Pulse: 110 beats/min
Temperature: 98.4°F
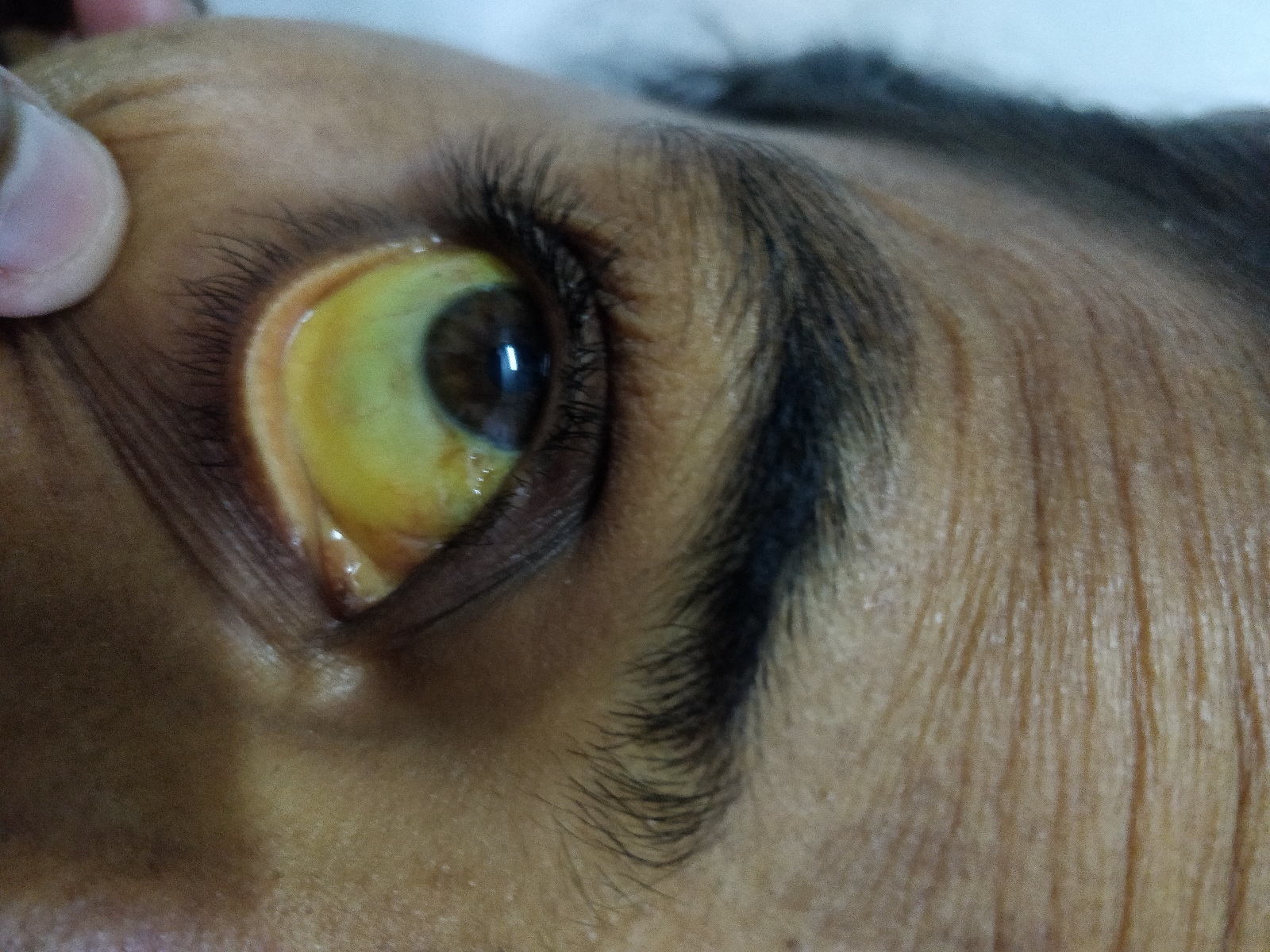
Yellowish discoloration of the conjunctiva, palms and legs are seen.
No pallor, cyanosis, clubbing, generalized lymphadenopathy, edema are seen.
Abdominal Examination:
1) Inspection:
Scaphoid, free flanks, umbilicus is midline and inverted.
No scars, sinuses, shiny skin, dilated veins.
No visible peristalsis.
2) Palpation:
No tenderness, no local rise in temperature
Hepatosplenomegaly is present.
Liver is present 3 cms in right hypochondrium, below the right costal margin in the mid axillary line. It is firm in consistency and smooth surface.
Spleen is in the left hypochondrium, enlarging towards the right iliac fossa, 6 cms below the left costal margin in the midclavicular line. It moves on respiration and has smooth surfaces.
No other palpable swelling was felt.
3) Percussion:
No shifting dullness, fluid thrill or puddles sign
Percussed through Nixons method.
4) Auscultation:
Bowel sounds were normal.
CVS:
S1 and S1 sounds were heard.
No murmurs.
Apical Impulse felt in the left 5th intercostal space, 1cm lateral to midline.
Respiratory System:
BAE, thoracoabdominal breathing
No added sounds.
Fever Chart:
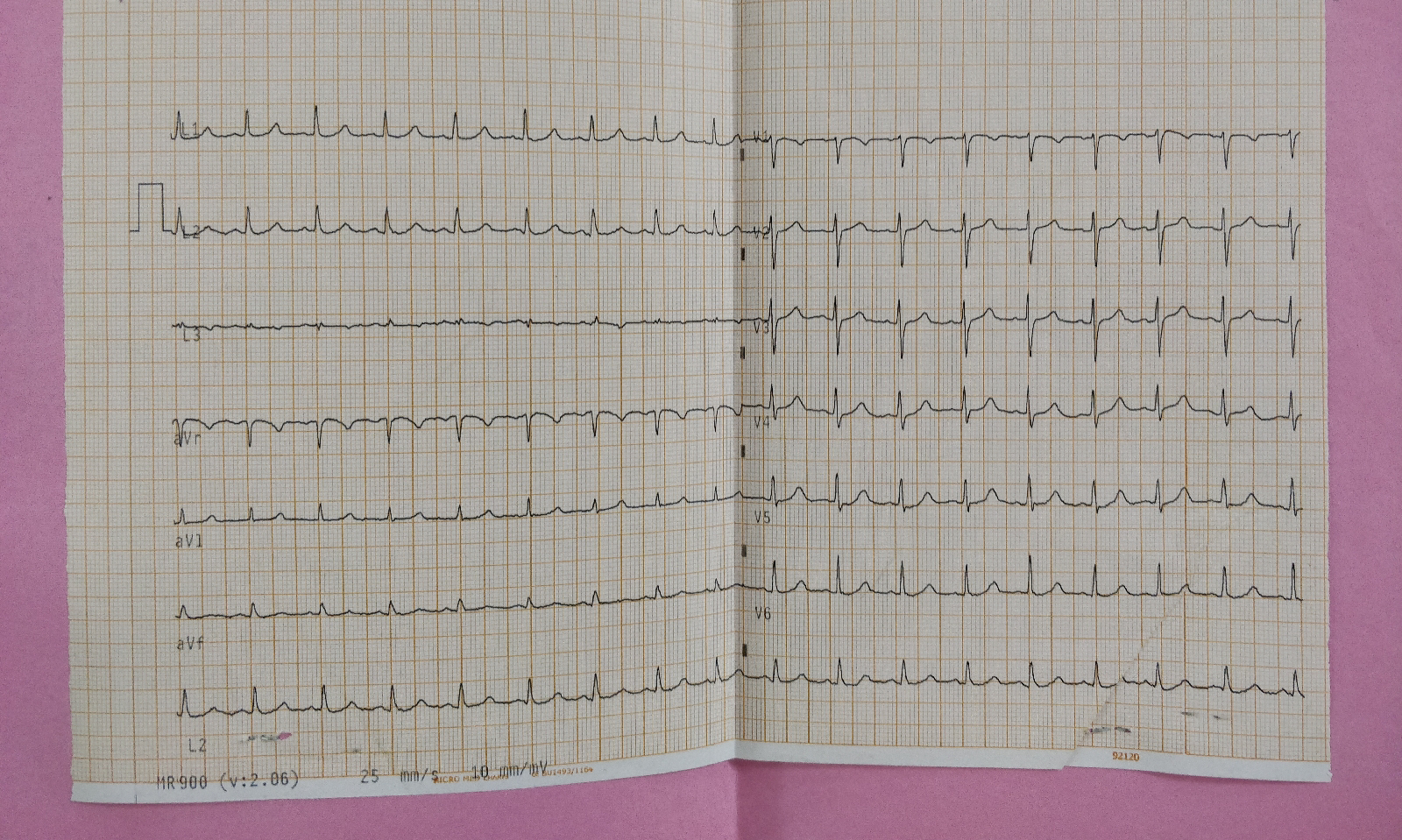
ECG:
X-ray:
Clinical Pictures:
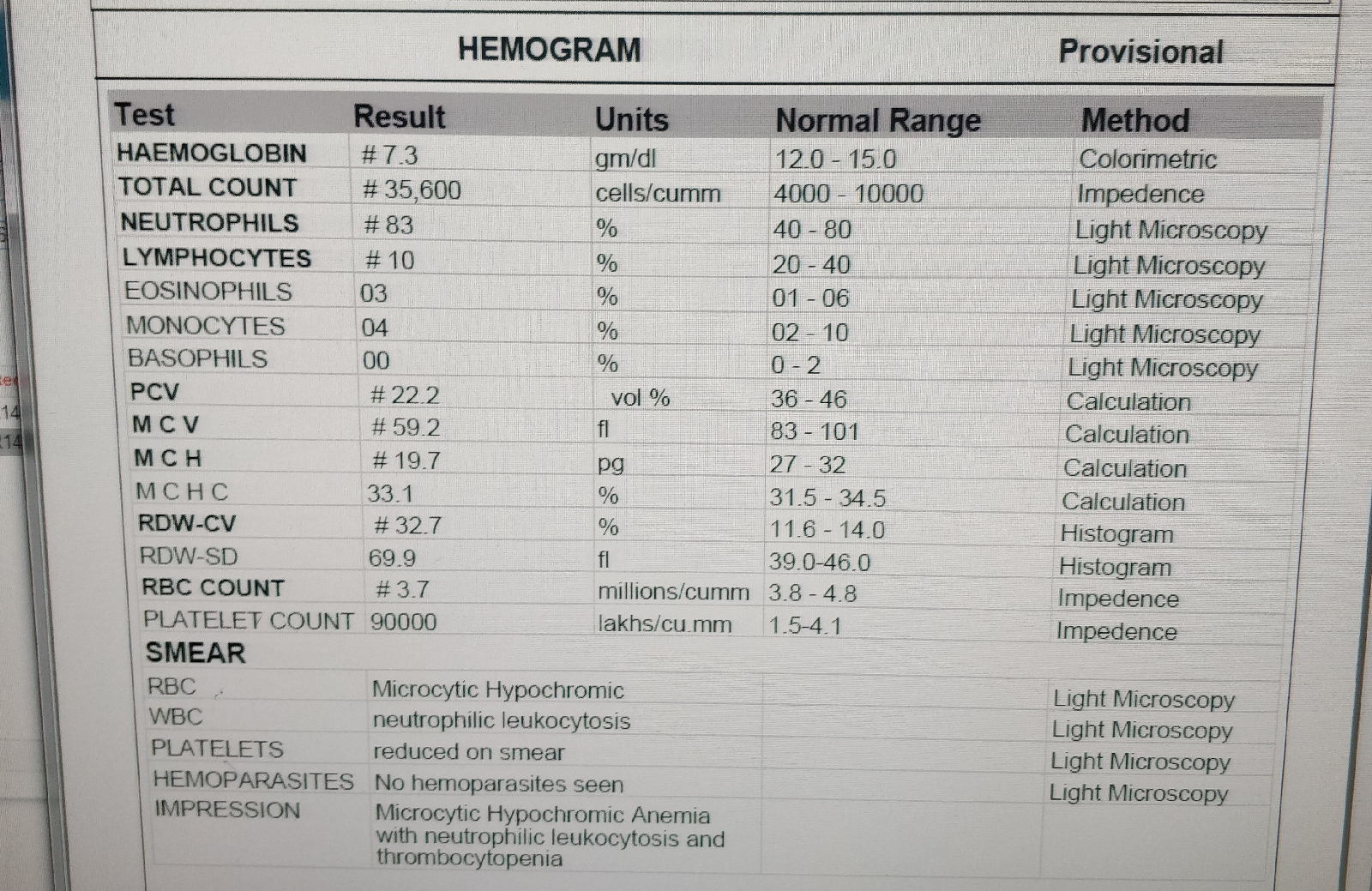
Lab investigations:
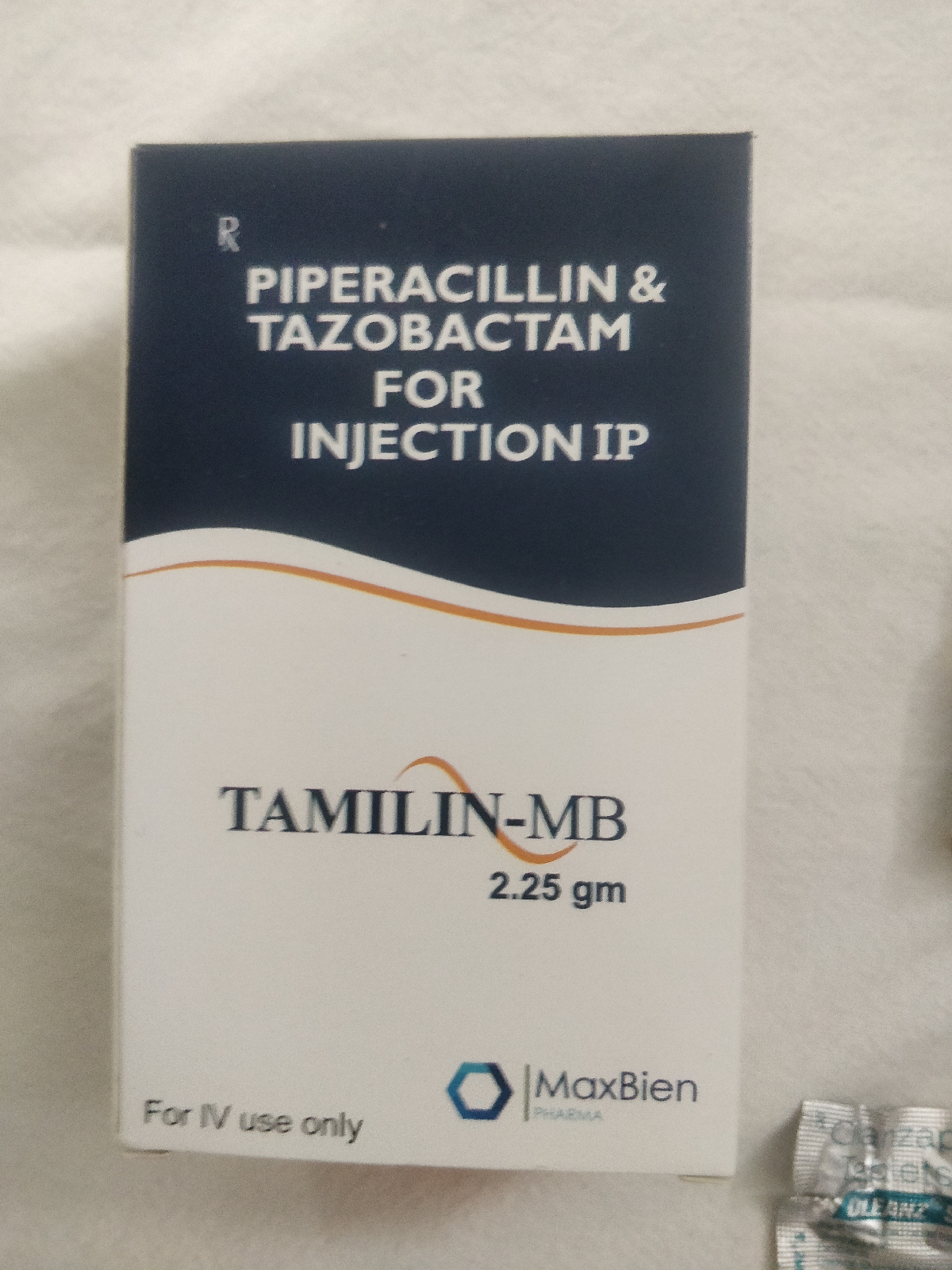
Treatment:


















Comments
Post a Comment